Endometriosis
By Dr. Christopher Ng
Obstetrician and Gynaecologist
GynaeMD Women’s & Rejuvenation Clinic, Camden Medical Centre
MBBS (London, UK), FRANZCOG (Aust-NZ), MMed (S'pore), FAMS (S'pore)
What is endometriosis?
What is endometriosis?
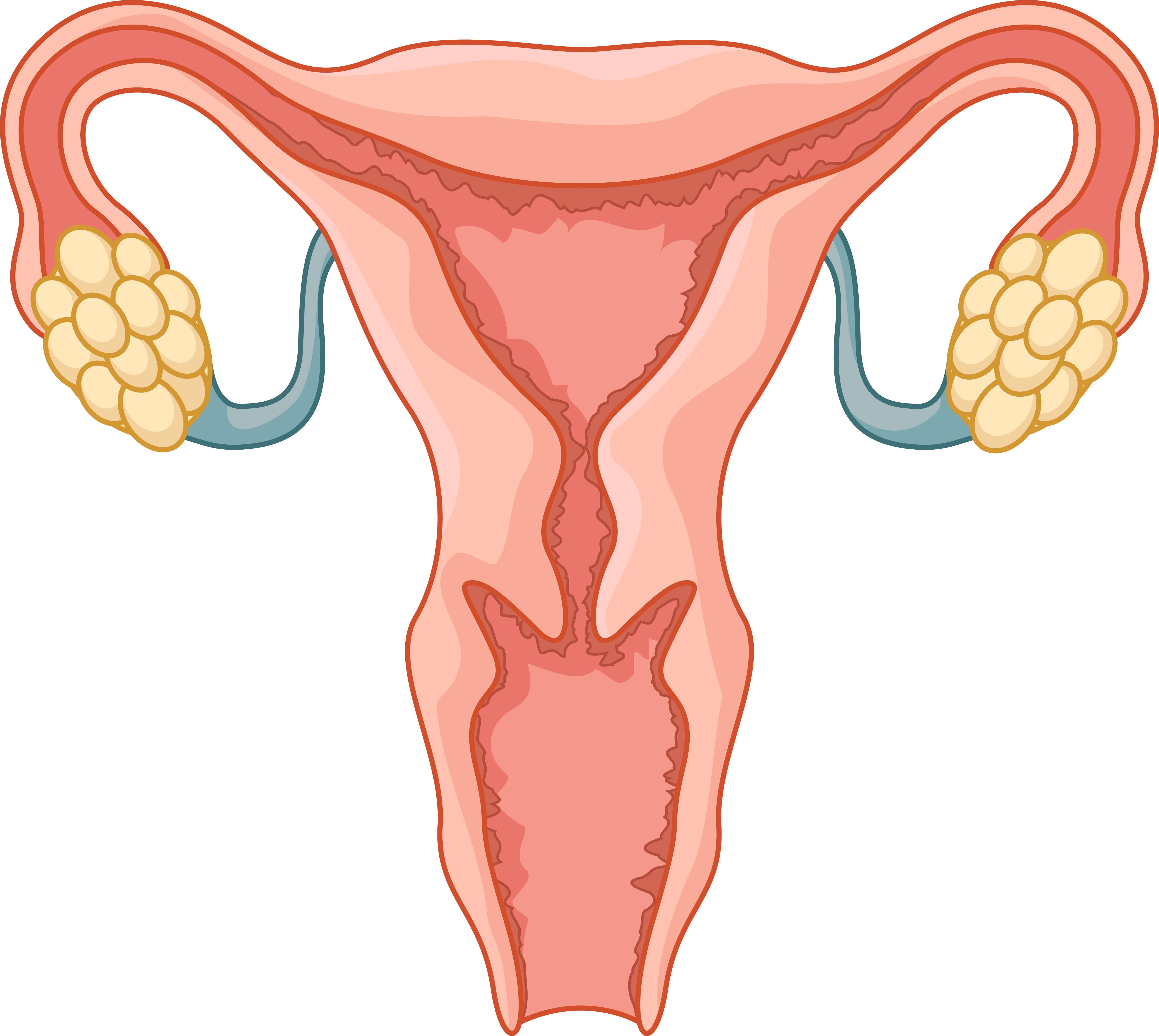
Endometriosis is a common medical condition characterised by growth of endometrium (the tissue that normally lines the uterus) beyond or outside the uterus. It looks and acts like tissue in the uterus. It most often appears in places within the pelvis:
- Ovaries
- Fallopian tubes
- Surface of the uterus
- Cul-de-sac (space behind the uterus)
- Bowel
- Bladder and ureters
- Rectum
Endometrial tissue can attach to organs in the pelvis or the peritoneum, which lines the inside of the pelvis and abdomen. In rare cases, it can also be found in other parts of the body. Endometrial tissue that grows in the ovaries can result in the formation of an endometriotic cyst.
Endometrial tissue outside the uterus responds to hormonal changes. During the menstrual cycle, it breaks down and bleeds similarly to the uterine lining. The breakdown and bleeding of this tissue each month can result in scar tissue known as adhesions.
Adhesions can cause pain and sometimes bind organs together.
The symptoms of endometriosis often worsen over time. In many cases, treatment can prevent the condition from worsening.
What causes endometriosis?
The causes of endometriosis are still unknown. People often think that this is because the blood from the period flows backwards into the pelvic cavity.

What are the signs and symptoms of endometriosis?
Women may complain of the following:
- Heavy and sometimes irregular menses
- Painful periods
- Pain during sex (this is a deep pain during penetration)
- Pain in the pelvis or lower abdomen in between periods
- It may be associated with infertility.
30–40% of women with endometriosis will have trouble getting pregnant after a year of regular sexual activity. Age-dependent cycle fecundity (monthly) rates in healthy fertile women range between 15% and 25%. That chance is less than 1% for women with severe endometriotic disease.
How common is endometriosis?
Endometriosis affects 5% to 20% of women of reproductive age and is the cause of infertility in 30 to 40% of women with endometriosis.

Is there a specific age group that is more susceptible to endometriosis?
It is more common in women between the ages of 20 and 40. According to the literature, Caucasian women are more likely than Afro-Caribbean women to develop endometriosis.
Is there a cure for endometriosis?
Endometriosis is hormonally related, so there is no permanent cure short of natural menopause or surgical menopause (by removing the ovaries); but even then, there are reports of endometriosis in menopausal women, though this is rare. There are, however, treatments available to help women manage and deal with their symptoms. In some women, pregnancy can alleviate the symptoms and effects of endometriosis. Endometriosis symptoms are usually lessened by pregnancy and hormonal drug treatments, but neither of these cures the disease.
Symptoms may or may not recur after childbirth. Breastfeeding can help most women postpone the return of symptoms, but only if it is frequent and intense enough to suppress the menstrual cycle. Doctors sometimes advise women with endometriosis not to delay having children because the condition tends to worsen over time. The longer you have endometriosis, the more likely you are to become infertile.

How is endometriosis diagnosed?
In addition to a thorough history, a pelvic exam will be done to see if you have any of the typical signs of endometriosis. This is done to try to pinpoint the source of the pelvic pain. Other potential causes of pelvic pain must be ruled out. Endometriotic cysts can be detected using a pelvic ultrasound scan, which is usually combined with a blood CA125 test (which can be high in women with endometriosis).
Endometriosis can be mild, moderate, or severe. A laparoscopy, also known as a keyhole surgery, can be used to look directly inside the pelvis to determine the extent of the disease. This procedure will be carried out while under general anesthesia. Endometriotic lesions, endometriotic cysts, and adhesions can all be removed during a laparoscopy.
What are the surgical and non-surgical treatment available?
Treatment focuses on either pain relief or infertility. Some pain relief options are as follows:
- Analgesics (Pain killer)
- Combined oral contraceptive pill
- Progression intrauterine device (Mirena)
- Danazol (Amle hormone compound)
- Oral progesterone (Visanne)
- Depot progesterone injections (Depoprovera)
- Gonadotropin-releasing hormone (GnRH) agonists — to create a tesendo menopausal state
They are all equally effective, but their side effects and cost profiles are different. Endometriosis-related pain is reduced when ovarian function is suppressed for several months with any of these medications.
Surgery may be recommended for some women whose medical treatment has not relieved their pain or infertility. Surgery is done to remove or coagulate all endometriotic peritoneal lesions, endometriotic ovarian cysts, deep rectovaginal endometriosis, and related adhesions, and to restore normal anatomy. Ablation of endometriotic lesions combined with removal of endometriotic adhesions improves fertility in endometriosis. Laparoscopic surgery nearly doubles the chances of pregnancy and live birth for women with mild endometriosis when compared to not having the surgery. Following surgery, pregnancy rates for women with mild endometriosis as their only fertility problem range between 81% and 84%. Those with moderate to severe endometriosis, including damage to the ovaries, have a 36% to 66% chance of getting pregnant after surgery. Endometriosis often comes back after treatment, so pregnancy rates are highest in the year after surgery.
Also, women who can't get pregnant after surgery may need SOIUI (superovulation intrauterine insemination) or IVF (in vitro fertilisation). SOIUI improves fertility in women with minimal to mild endometriosis, but tubal patency is required. IVF is a good treatment option, especially if the tubes are blocked, if male factor infertility is present, or if other treatments haven't worked.
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
