Reducing breast engorgement with cabbage leaves & gel packs
Reducing breast engorgement with cabbage leaves & gel packs
By Dr Wong Boh Boi
Founder and Senior ParentCraft Consultant

Breast engorgement is one of the common problems experienced by mummies after the birth of their children. It is the feeling of tightness in your breast that can result in hardness and pain. There are multiple theories behind this phenomenon, and the most popular belief is that there is an increase in milk production. If you have it, you are not alone. In fact, studies have found that 20–70% of women experience breast engorgement.1,2
There have been many traditional methods that have been explored in the past, including methods like breast massage.
To help relieve these common symptoms, Dr Wong experimented with the use of cabbage leaves and cold gel packs.3 The study was published in the top international nursing journal (International Journal of Nursing Studies). We would like to share the findings of the study in this article.

How was the study conducted?
A randomised controlled trial was conducted, and 227 mothers were divided into three groups:
Group 1: Cold cabbage leaves application plus routine care by the hospital
Group 2: Cold gel packs application plus routine care by the hospital
Group 3: Control group which received routine care by the hospital only
*Routine care includes education on breastfeeding during antenatal classes, daily in-house postnatal teaching classes, and during rounds conducted by lactation consultants. Lactation consultants also help to rectify problems during breastfeeding. Pain management may include: 1) Paracetamol 500mg (two tablets of 250mg) three times a day; 2) Synflex 550mg (2 tablets of 275mg) two times a day; or 3) Ponstan 500mg (2 tablets of 250mg) three times a day.
This was the study flow and data collection point
The first application of cabbage leaves or gel pack
a. Data collection after 30 minutes
b. Data collection after 60 minutes
c. Data collection after 120 minutes
The second application of cabbage leave or gel pack
a. Data collection after 30 minutes
b. Data collection after 60 minutes
c. Data collection after 120 minutes
Results
Cabbage leaves were found to be most effective in relieving pain and hardness. Gel packs were also helpful to some extent. Mothers who used cabbage leaves were most satisfied, followed by those who used gel packs.
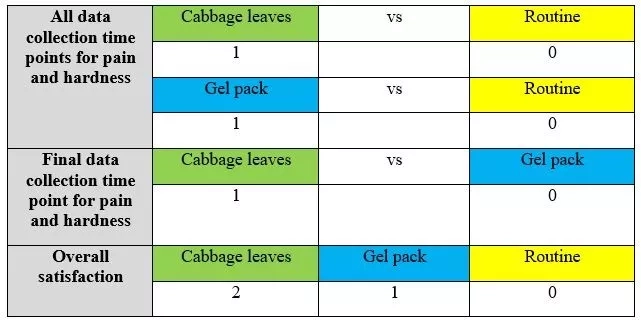
Total scores for the 3 groups:
Cabbage leaves – 4 points
Gel packs – 2 points
Routine care – 0 point
Now we know that cabbage leaves are most effective, let us teach you how to apply the cabbage leaves.
- The cabbage leaves can be the common green cabbages (Brassica oleracea).
- Remove the hard stem of the cabbage leaves.
- Rinsed the cabbage leaves in cold water and chill in the freezer for 15 minutes in a zip lock freezer bag or in the fridge for 1 hour before application.
- Apply 3 big leaves (preferably the outmost leaves) on top of each other on each breast, and cover the entire breast with the leaves. Support the leaves by wearing a bra.
- Leave it on for two hours, or until the cabbage loses its coldness. You may use a new set of cabbage leaves thereafter.
- Eat the rest of the cabbage! ?
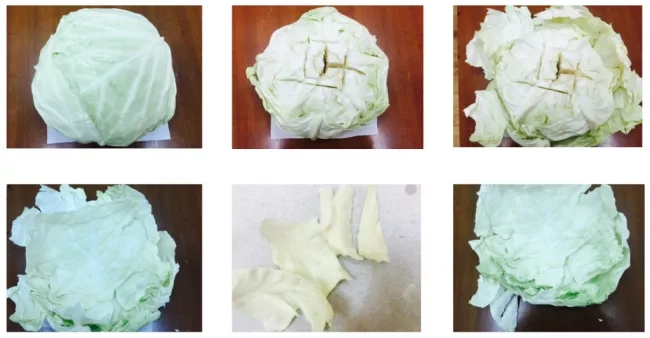
Cabbage leaves preparation

How does cabbage leaves help to reduce breast engorgement?
There is no definitive answer to this. However, we hypothesise that it is due to cabbage leaves containing enzymes such as sinigrin and rapine, which have proven to be a good source of antioxidants.3,4 The sulfur compound in cabbage leaves has antiseptic, disinfectant, antibacterial, and anti-inflammatory properties, which may support their use to ease pain and swelling.6 Having the cabbage leaves chilled can also increase its effectiveness.7
References
1.Spitz IM, Bardin CW, Benton L, Robbins A. Early pregnancy termination with mifepristone and misoprostol in the United States. N Engl J Med. 1998, 338(18), 1241-1247.
2. Walker M. Breastfeeding and engorgement. Breastfeeding Abstracts. 2000, 20 (2), 11-12.
3. Wong BB, Can YH, Leow MQH, Lu Y, Chong YS, Koh SSL, He H. Application of cabbage leaves compared to gel packs for mothers with breast engorgement: Randomised controlled trial. International Journal of Nursing Studies. 2017; 76: 92-9.
4. Joy J. A study to evaluate the effectiveness of chilled cabbage leaves application for relief of breast engorgement in volunteered postnatal mothers who are admitted in maternity ward of selected hospital in Belgium. 2013. Masters’ thesis. KLE University.
5. Nilnakara S, Chiewchan N, Devahastin S. Production of antioxidant dietary fibre powder from cabbage outer leaves. Food Bioprod Process. 2009, 87 (4), 301–307.
6. Hatfield G. Encyclopaedia of folk medicine: old world and new world traditions. 2004. ABC-CLIO, California. pp. 59-60.
7. Rosier W. Cold cabbage compresses. Breastfeed. 1988. Rev 12, 28-31.
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
Quick guide to morning sickness in pregnancy
Quick guide to morning sickness in pregnancy
By Dr. John Yam
Obstetrician & Gynaecologist
MBBS, FRCOG, MMED, FAMS

"Morning sickness" is a term used to describe the nausea and vomiting that occur during pregnancy. It affects about 75% of pregnant women and, despite it being called morning sickness, it can happen at any time of the day.
The good news for most expectant moms is that morning sickness is mild and tends to get better during the last 12 to 14 weeks of pregnancy. But there are some women who have it for a longer time, and sometimes they have it the whole time they are pregnant.
Hyperemesis Gravidarum is a severe form of morning sickness that only a small number of women who are expecting get. It is a condition where nausea and vomiting are so severe that they cause dehydration, resulting in the loss of more than 5% of the pre-pregnancy body weight. Hyperemesis gravidarum may require hospitalization and treatment with intravenous (IV) fluids and medications.
In most cases, morning sickness is mild and does not require any treatment. An expectant mother’s experience with morning sickness will vary. The symptoms can vary between pregnancies as well; while you might experience severe symptoms in one pregnancy, the next one might be a breeze!
COMMONLY ASKED QUESTIONS:

1. What causes morning sickness?
There is no known single cause. Many factors could play a part in triggering the feeling of nausea. Some people think that the rising level of the pregnancy hormone (hCG) is one of them. Higher levels of the hormones estrogen and progesterone, as well as reduced blood sugar, may also aggravate symptoms.
Other factors and triggers include:
- Sensitivity to smell: you could keep tabs on what triggers your symptoms and try to avoid these triggers
- Pre-existing motion sickness: this could worsen during pregnancy
- Stress can initiate or aggravate digestive issues
- Physical and mental fatigue
- Certain medical conditions could be associated with increased symptoms of nausea, such as thyroid issues, urinary tract infections
- If you are pregnant with more than one baby, chances are you could have more than your share of symptoms than you might have had if you were carrying just one

2. Will that affect my baby's growth?
You may not be feeling your best, and you may not be eating as much as you did before pregnancy, but this is usually not a problem.
In the first trimester, your baby gets most of her nourishment from your body’s reserves. Retching and vomiting will not cause any physical harm to the baby, and your appetite should improve by the end of the first trimester.
However, if you have lost more than 5% of your pre-pregnancy weight and your appetite has not picked up (not able to eat or drink anything), it is imperative to consult your doctor.

3. Any tips to cope with it?
Every woman has a different experience with morning sickness. There is no one-size-fits-all solution. However, lucky for you, there are some ways to alleviate the symptoms.
a. Diet
- Stick to foods & beverages that appeal to you for now. Avoid eating, smelling or even thinking of foods that may trigger the nausea. Even if that means you might be eating the same few dishes frequently.
- Eating small, frequent meals at regular intervals may help to ease the symptoms.
- Eat early! Morning sickness may kick in the moment you are out of bed or even when you are brushing your teeth in the morning. Nausea is likely to strike when your tummy is empty after a long night’s sleep. Try to stock up some healthy snacks like cereals, crackers or nuts by your bedside so you have something to munch on the moment you open your eyes.
- Try a light, healthy supper before bed. Try snacking on complex carbs and something high in protein – e.g. Whole grain meal, a glass of milk, almond nuts, freeze dried fruits.
- Eat nutrient-dense foods! Plan your diet to include protein and complex carbohydrates.
b. Fluid
It is important to get sufficient fluids. Drink plenty of fluids at regular intervals to avoid dehydration. If water is not appealing to you, try sucking on a popsicle instead. Fruit juices are a tasty alternative too.
c. Supplements
Take your prescribed prenatal vitamins. These will help compensate for any nutrients that may be lacking.
d. Ginger
A traditional folk remedy that has stood the test of time. Sucking on fresh or preserved ginger slices, sipping on ginger ale, or even a cup of ginger tea might ease the queasiness.
e. Acupressure wristbands
Some pregnant women swear by the effectiveness of these. This drug-free solution has no side effects and is available at most pharmacies.
f. Get plenty of rest
Nausea gets worse with fatigue and stress.
g. Get help from your obstetrician
Keep anti-sickness medicine on standby in case you feel unwell.
4. Is my pregnancy normal if I have no morning sickness?
Not all expectant mums experience morning sickness, so lucky for you. There is no way to tell if a pregnancy is normal based on whether or not a woman has morning sickness.
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
How to choose a maternity insurance plan?
How to choose a maternity insurance plan?
Every couple wishes for a smooth, safe pregnancy and delivery of their baby. However, they might be worried about the complications at birth and other concerns that may instill the purchase of maternity insurance. Here is a list of some information that you might find useful in the course of finding a suitable one.

What is maternity insurance and are there different types?
There are basically two types of maternity insurance that will cover an expectant mother during her pregnancy journey:
- Covers the costs of delivery
Maternity insurance covers the costs of delivery. However, the coverage varies from individual to another individual. You would expect to pay a hefty price tag for one that requires higher coverage, such as a rider or an international medical plan for expats. Comparing this to our local integrated plans (IP) or group insurance provided by your employers, prices would be more affordable. However, do take note that the coverage does differ. - Covers the costs of specific pregnancy complications and congenital conditions
Larger life insurers such as AIA, AXA, GE and Prudential would be able to cover mothers for pregnancy complications and congenital disorders. Alternatively, you automatically receive such free coverage if you decide to store your child’s cord blood with Cordlife.

What does maternity insurance cover?
- Common conditions
Maternity insurance covers common complications and conditions for both mother and child that will require treatments which are not normally covered by their personal medical insurance or employee benefit insurance. The common child congenital conditions are Down syndrome, cerebral palsy or cleft lip. As for mothers, the common complications covered are pre-eclampsia/eclampsia and amniotic fluid embolism. - Common pregnancy complications
Maternity insurance also covers common pregnancy complications like pre-eclampsia, which accounts for 63% of pregnancy complication claims and 16% for abruptio Placentae. Moreover, not only are mothers covered under maternity insurance, your little one will be covered for common child congenital conditions such as heart conditions which makes up 40% of the claims.

What are the considerations in choosing maternity insurance plans?
The plans available in the market are generally similar, below are some of the considerations:
- Coverage:
a. Sum assured: Most plans cover between $5,000 to $10,000, except for AIA which you can choose coverage of up to $25,000.
b. Scope of cover: Most plans cover 7-10 types of pregnancy complications and 17-18 types of child congenital conditions, but again AIA covers up to 14 and 25 conditions, respectively. Most plans will come with a hospital cash benefit, that will pay $100 per day of hospital stay.
c. Length of cover: All plans start the coverage from 13 to 18 week of pregnancy and terminates when your child turns 2 to 3 years old. - Premium:
a. The premium costs hover around the same range: Starting from the lowest $315 to $395. A $5,000 coverage is for options that require you to purchase a regular premium whole life plan or investment link plan. GE is the only insurer with a plan that does not require a client to get a whole life plan and premium starts from $542. Cordlife’s plan is complimentary if you decide to sign up their cord blood banking services. - Other features:
a. Underwriting: All plans require the insured individual to complete health declarations and scans of foetus, except for Cordlife’s. Their coverage will start automatically after 18 weeks of pregnancy and as soon as you enrol in their services.
b. IVF pregnancies and babies are only covered by AIA and Cordlife’s plan.

Which plan should I pick?
Everyone's perspective and situation would be unique. Here’s our friendly advice—select a plan based on these two options:
- Plans with the best value
The plans are complimentary if you have decided to sign up for Cordlife’s cord blood banking service. This makes it the best bang for buck. The coverage may not be one of the highest in the market, but a coverage of six months is more than sufficient as most congenital conditions would be diagnosed by then. In addition, with no underwriting as a requirement, it would be a useful and convenient feature as it could be time consuming to submit all medical requirements. - Plans with the highest coverage
Go for AIA’s Mum2baby, as it has the highest sum assured option – $25,000. Furthermore, it covers the most type of pregnancy complications and congenital conditions.
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
Tips for pregnant mothers during COVID-19
Tips for pregnant mothers during the COVID-19 pandemic
By Dr Ng Ying Woo
Obstetrics & Gynaecology

Pregnancy is often a joyous event in our lives. However, this has been dampened by the recent COVID-19 pandemic. The disease has spread to almost every part of the world, including Singapore. Drastic measures such as circuit breaker and social distancing have been implemented in our country. These measures have brought stress and uncertainty to our expectant mothers. Thus, it is natural that most mothers have questions about the disease and how it impacts their pregnancy.
Here are some tips that may help you to ride safely through this pandemic:
Is it safe to go for my prenatal check-ups?
These check-ups are essential during your pregnancy. The risk of contacting the virus is probably low as hospitals and clinics scan the temperature of every visitor, and there are hand sanitisers at almost every counter. Wearing masks, keeping a safe distance from others, and driving directly to the hospital instead of taking public transportation may help reduce the risk of contact even more.
What should I do as a pregnant mother to keep myself safe from COVID-19?
Stay home to minimise the risk of infection. Going out to shop for baby stuff like we used to may not be advisable. Pregnant mothers may need to adjust their preparation and make purchases online instead.
You might have to do most of your prenatal workouts at home if you want to stay healthy and fit before giving birth. Precautions like these should help pregnant mothers to stay safe and well from COVID-19.
How will the new precautionary measures in place at hospitals affect me?
Congratulations! You and your loved ones have gotten through the circuit breaker period safely. From June 2, 2020, Singapore has entered Phase One of reopening:
Husbands with negative contact history will continue to be allowed to accompany their wives during active labour. However, everyone in the labour room will still have to wear masks.
In Phase 1, a maximum of five pre-designated visitors will be allowed to visit inpatient wards. However, only one person will be allowed to visit the patient at a time. Children below 12 years old are still prohibited from visitation. Though the family may be excited to visit the new mother and baby, be sure to remind them of this visitation restriction.
Is it still safe to give birth in a hospital with the current situation?
The hospital has strict rules about keeping people from getting sick and keeping infections under control. Measures such as temperature scans, health declarations, mask wearing at all times, frequent use of sanitisers, restriction of visitation, etc. help to keep the risk COVID-19 spreading to our mothers to a minimum.
How should I prepare for my stay in the hospital? Are there additional items I should pack in my hospital bag?
Simple preparations such as clothing for yourself and the baby should suffice. Your husband can help to prepare the required documents and other miscellaneous items, e.g. camera, mobile phone charger, etc.
With consideration of COVID-19, a small bag of masks and hand sanitiser may be useful.
Stay strong and stay together
Use a positive outlook and attitude to deal with the worries and fears that this pandemic has caused. With that in mind, we can safely welcome our little one into our family.
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
Essential birth planning tips
Essential birth planning tips

Written By: Dr. Edwin Thia
Senior Consultant
The Prenatal Consultants
Mount Elizabeth Novena Specialist Centre
You are now in the third trimester. This is the best time to talk about birth plans with your doctor. Birth planning includes discussing about your preferred mode of delivery, what forms of pain relief available during delivery, how you want to approach your delivery, the immediate after care for you and your newborn baby, whether you would like to store your baby’s cord blood etc.
Mode of delivery
We start by discussing the two modes of delivery – vaginal delivery and caesarean section.
All women are encouraged to have a vaginal delivery if there are no medical or obstetrical reasons to exclude this. Most women will go into labour on their own around week 39, and they will have a normal vaginal delivery that goes well.
Labour
Labour is traditionally divided into three stages:
Stage 1
The cervix begins to dilate and is made up of two phases—a latent phase and an active phase. The latent phase is when the cervix dilates and thins out to about 3 cm. This stage is often very variable in duration and can last from a few hours to a few days. The symptoms are usually not specific and can range from mild abdominal cramps, backaches, or the passing of some bloody mucus discharge (show). Some women may not have any symptoms at all.

The active phase is when the cervix continues to dilate and thin out to be fully dilated (about 10 cm). The typical rate of dilation in the active phase is about 1 cm per hour, and hence the average duration is about 8 to 10 hours. This phase is when you have painful, regular contractions. The contractions are much more painful and more frequent, and each contraction usually lasts for up to 30 to 45 seconds. Your uterus is actively working to dilate and thin out the cervix.

Stage 2
This stage involves the delivery of your baby. This is when you have to work the hardest to push your baby out. This stage may last from 30 minutes to up to 2 hours. You will usually have a sensation and an urge to bear down due to the pressure of the baby’s head on your perineum. Your legs may be raised to allow more room for the baby. An episiotomy may sometimes be needed to increase the space.
Stage 3
The placenta is expelled at this stage. This usually lasts between 5 and 30 minutes. Your uterus continues to contract and will squeeze out the placenta after it detaches from your uterus.
Pain relief during labour
Pain is expected during labour, and there are various methods of pain relief available to you. The three most common pain relief methods are Entonox gas, opioid injections, and epidurals.
Entonox is an inhalational form of analgesia. The mother breathes in a gas mixture of 50% nitrous oxide in oxygen. Entonox doesn't get rid of pain; it just changes the way you think about it so that it hurts less. The effectiveness is about 50%.
An opioid injection is a type of drug that is injected into the muscle of the thigh and provides pain relief for about 3 to 4 hours. It cannot be given too close to the delivery of the baby because it can make the baby drowsy at birth and cause temporary breathing problems. It can reduce pain by up to 70%, but only for a short duration of about 3 to 4 hours.
Epidural is the most effective and reliable pain relief method. This is done injecting an anaesthetic medicine into a space within the spinal canal. This is done by a trained anaesthetist. The epidural can last throughout the entire duration of the labour. If an emergency caesarean section is required, it can also be used for the operation.
Instrumental delivery
Instrumental delivery is sometimes needed to help a vaginal delivery go smoothly. This can be done either using a vacuum suction device or forceps. There can be many reasons for needing help with the birth of your baby. Some common reasons are if you are not able to push well during the second stage of labour or if there are concerns with the well-being of your baby.

Caesarean section
If you can't give birth through the birth canal, you will need a caesarean section. Depending on your situation, you can choose to have a planned caesarean section or you may need an emergency caesarean section.
A planned elective caesarean delivery is often done because the baby is in the wrong position or the placenta is low. Reasons for an emergency caesarean delivery include fetal distress during labour or slow progress of labour.
Caesarean delivery is considered a major operation. Although generally a safe operation, there are some risks involved, like any other major surgical operation. Most women who have a caesarean section will recover well. However, there are risks for both you and your baby, and it may take longer for you to get back to normal after your baby is born. Having a caesarean section also makes future births more complicated. The main risks associated with having a caesarean section include wound infection, more bleeding than expected, and blood clots in the legs (deep vein thrombosis) that can travel to the lungs (pulmonary embolism). Future pregnancies will be seen as higher risk, which may change how your next pregnancy is cared for.
Deferred cord clamping
After your baby is born, the umbilical cord is clamped and cut before the placenta is expelled. Deferred or delayed cord clamping provides the newborn baby with an additional 80-100 mL of blood. The cord is not clamped in the first 60 seconds, except where there are concerns about the cord integrity or if the baby’s heart rate is abnormal. This additional blood improves the iron stores in the baby’s infancy.
Cord blood banking
If you choose cord blood storage, it will be collected after your baby is born but before the placenta separates from your womb. Cord blood collection does not interfere with delayed cord clamping.
Some of your baby’s cord blood will also be collected for specific laboratory testing like blood grouping, thyroid function tests, and glucose-6-phosphate dehydrogenase (G6PD) deficiency testing. After that, cord blood can then be collected for cryogenic storage.
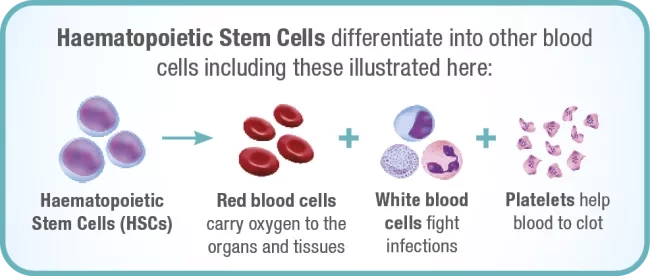
Cord blood banking is the process of storing your baby’s umbilical cord blood in the umbilical vein. Your baby’s umbilical cord blood stem cells are a rich source of haematopoietic stem cells (HSCs), which are responsible for replenishing the blood and regenerating the immune system.
In addition, HSCs are also known as naive precursor cells as they have a unique ability to differentiate into the different types of cells found in the body, namely: red blood cells, white blood cells, and platelets.
When parents decide to store their baby’s cord blood stem cells, they will be availing their baby (and family) of the following possible benefits:
1. Mainstream treatment of over 80 diseases ranging from leukaemia, lymphoma, thalassaemia as well as metabolic and immune disorders.1 There are currently clinical trials underway for the possible treatment of Cerebral Palsy, Autism, Type 1 Diabetes, Alzheimer’s disease and spinal cord injury and many more.2
2.A sure match for autologous (donor and recipient are the same person) transplants. Since cord blood stem cells are "naive," they can change into different types of cells and do not need to be a perfect match like bone marrow transplants do. There is also a 40–60% chance of a match between siblings.3 So, parents are strongly encouraged to save for each child because it makes it more likely that they can cover each other if they need to.
3. Lower risk of Graft-versus-Host Diseases (GvHD) for autologous transplants, which makes it less likely that a stem cell transplant will be rejected.
4. A ready supply of life-saving stem cells that can be used quickly in a transplant situation where time is of the essence. Unlike bone marrow, which requires a perfect match between donor and patient, the probability of finding a match among family members using cord blood stem cells is higher.
When it comes to collecting your baby’s cord blood, it will be done by your OBGYN doctor. This process usually takes less than 5 minutes and is a safe and risk-free procedure for both mother and child.
Skin to skin contact
After your baby has been cleaned up, he/she can be laid directly on your bare chest, and both of you are then covered with a warm blanket. This helps to calm and relax both you and your baby. It also helps to regulate the baby’s heartbeat and breathing, helping them better adapt to life outside the womb.

Conclusion
You should be all ready for the birth of your baby. Your doctor will now continue to monitor your pregnancy's well-being. Your doctor will also be doing a vaginal swab soon to check for the presence of Group B Streptococcus and will continue to monitor the growth and well-being of your baby.
Keep going to your regular appointments, and here's hoping that your birth plans go as planned.
References:
1 For the full list of treatable diseases and references, please refer to https://www.cordlife.com/sg/treatable-diseases.
2 Diseases and Disorders that have been in Clinical Trials with Cord Blood or Cord Tissue Cells page. Parent’s Guide to Cord Blood Foundation website. https://parentsguidecordblood.org/en/diseases#trial. Accessed March 8, 2021.
3 Beatty PG, Boucher KM, Mori M, et al. Probability of Finding HLA-mismatched Related or Unrelated Marrow or Cord Blood Donors. Human Immunology. 2000; 61:834-840.
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
Pagination
- Previous page
- Page 3
